On this page...
Introduction
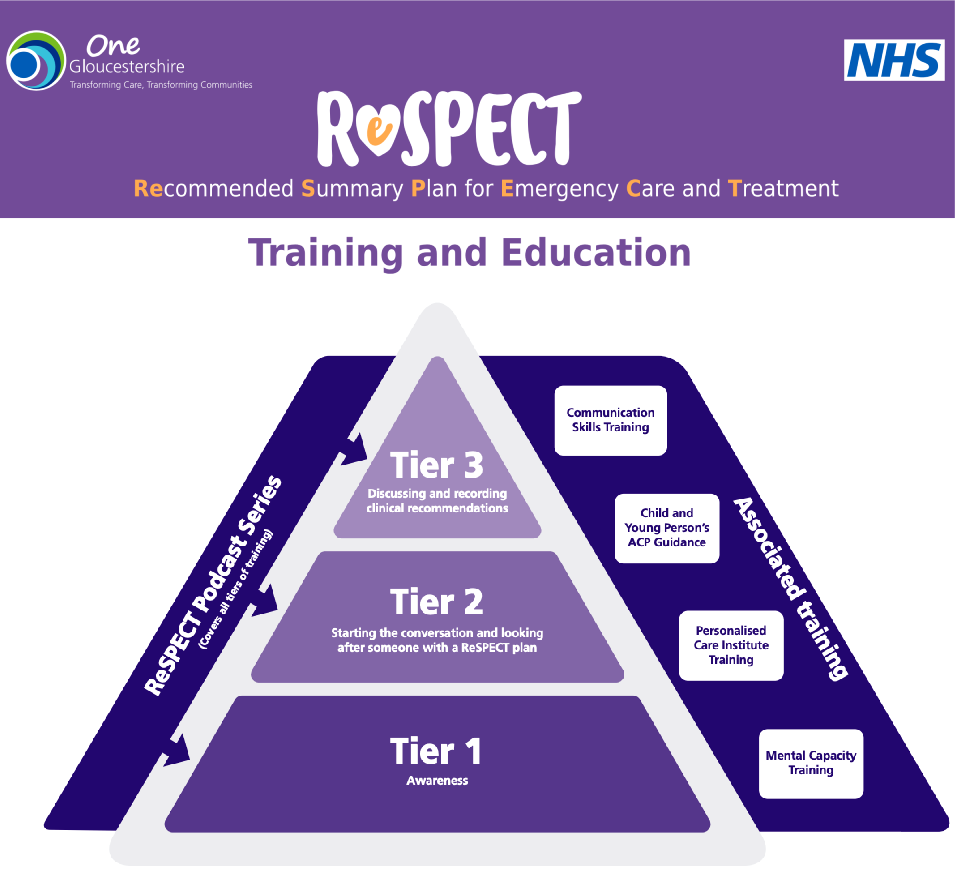
Which Tier of training do I need?
To identify which tier of training you need to access for your role, use the table in the link below, then scroll down to reach the appropriate tier.
For further information about using the ReSPECT training framework please watch this introductory video (Coming Soon)
Learning Objectives
Each tier of the framework has a set of learning objectives. Any teaching provided for that tier should cover the objectives to ensure the relevant information is covered.
To access the learning objectives please follow the links below.
Tier 1 training resources
To complete Tier 1 training, it is recommended that you complete the following 4 activities:
- Review the ReSPECT plan specimen plan. ReSPECT_v3-1_Form_Specimen_FINAL.pdf
- Watch the video “Joe’s ReSPECT journey” (6 minutes). Joe’s ReSPECT Journey – a ReSPECT explainer for healthcare professionals
- Watch the Tier 1 awareness session recording for staff. (Coming Soon)
- Discuss ReSPECT with your team – Understand the local processes for supporting ReSPECT within your team and how your role can support this important work.
Further information supporting Tier 1 can be found at the links below:
| Webpage link | Resuscitation council – ReSPECT for health care professionals | ReSPECT for healthcare professionals | Resuscitation Council UK |
Tier 2 training resources
To complete Tier 2 training, it is recommended that you complete the following 4 activities:
- Tier 1 resources (as applicable to increase knowledge related to role).
- Watch the video “ReSPECT conversations – An update for healthcare professionals”. ReSPECT Conversations – An update for healthcare professionals
- Watch the Tier 2 session recording. (Coming Soon)
- Discuss ReSPECT with your team – Understand the local processes for supporting ReSPECT within your team and how your role can support this important work.
Further information supporting Tier 2 can be found at the links below:
| Paper Resources | Resuscitation Council Leaflet “The ReSPECT process – A guide for clinicians completing the plan” (sections 1-3 only) | ReSPECT Guide for Clinicians_FINAL.pdf (resus.org.uk) |
| Gloucestershire – Ask and check poster for care homes | Ask-Check-Poster-Care-Home_25.pdf | |
| Gloucestershire – ReSPECT top tips | UPDATED ReSPECT_Top_Tips_A4_Nov25-final.pdf | |
| Resuscitation Council – Information for care homes – FAQ’s | ReSPECT Information for Care Homes_FINAL.pdf (resus.org.uk) | |
| Resuscitation Council – Information for the ambulance service | ReSPECT_Ambulance Service v4_08-2023-2.pdf | |
| Generic myth busting document | (Being Updated) |
Tier 3 training resources
To complete Tier 3 training, it is recommended that you complete the following 4 activities:
- Tier 1 resources (as applicable to increase knowledge related to role).
- Tier 2 resources (as applicable to increase knowledge related to role).
- Watch the Tier 3 session recording (1 hour) Understanding and Completing ReSPECT
- Attend a Community of Practice online session – these sessions will be led by a clinician experienced in the ReSPECT process and will allow the opportunity to discuss experiences, practice conversations and ask questions. Community-of-Practice-poster.docx
Further information supporting Tier 3 can be found at the links below:
| Paper Resources | Resuscitation Council – The ReSPECT process – A guide for clinicians completing the plan | ReSPECT Guide for Clinicians_FINAL.pdf |
| Resuscitation Council – 10 top tips for GPs | ReSPECT Ten Top Tips_FINAL.pdf (resus.org.uk) | |
| Revamp your ReSPECT discussions poster | ReSPECT aide memoire v1.2 Gloucestershire | |
| Publication – decisions relating to CPR | Publication: Decisions relating to cardiopulmonary resuscitation (3rd edition – 1st revision) | Resuscitation Council UK |
ReSPECT Policy
All health and care professionals involved in the ReSPECT process should refer to the One Gloucestershire ReSPECT policy for use across all
providers in Gloucestershire.
Gloucestershire-ReSPECT-Policy-Sept-2025final-pdf.pdf
Gloucestershire ReSPECT Podcast Series
Welcome to our short podcast series where we discuss all things ReSPECT! Our wonderful host Tanya de Weymarn, Emergency Medicine and Frailty Consultant and Clinical Lead for End of Life for the ICB and self-proclaimed ReSPECT enthusiast, is joined by various health and care staff working across Gloucestershire throughout these 6 episodes to breakdown what ReSPECT planning is, how to complete ReSPECT plans otherwise known as the ‘Purple form’, as well as the benefits and misunderstandings of ReSPECT. There will be useful phrases, myth busting, good practice top tips and much more…
The ReSPECT Podcast Series – YouTube
ReSPECT Audit
- Countywide Audit Tool – Developed to support ReSPECT audits in health and care settings Gloucestershire. ReSPECT-Audit-tool-Gloucestershire-v3-July-25.xlsx
- Resuscitation Council – Criteria for auditing and evaluating the ReSPECT process and suggested measures for service evaluation in Secondary/Tertiary care. ReSPECT audit service evaluation and patient experience questions.pdf
Resource List for patient and carers
ReSPECT-public-and-carer-information.pdf
Appendix: Other training and resources that can support the ReSPECT process

